How To Lower Cholesterol: Know Your Fats
The American Heart Association recommends that just 25% to 35% of your daily calories come from fats such as those found in fish, nuts, and vegetable oils. For healthy people, saturated fat should comprise no more than 7% of your total calories. On a 2,000 calorie-a-day diet, that’s about 140 calories worth of saturated fat. If you need to lower your LDL cholesterol, limit saturated fat to 5% to 6% of calories, or about 11 to 13 grams of saturated fat on a 2,000-calorie diet. Reduce trans fats to less than 1% of your total daily calories. This means avoiding fried foods and many junk foods.
Strategies To Control Plasma Triglycerides
Although CVD risk is increased when fasting TGs are > 1.7 mmol/L , the use of drugs to lower TG levels may only be considered in high-risk patients when TGs are > 2.3 mmol/L and TGs cannot be lowered by lifestyle measures. The available pharmacological interventions include statins, fibrates, PCSK9 inhibitors, and n-3 PUFAs. A meta-analysis of 10 trials included people treated with various agents that reduce serum TGs and reported a 12% reduction in CV outcomes. Recently, the REDUCE-IT trial demonstrated that in statin-treated patients with high CV risk with fasting TG levels between 135499 mg/dL , high-dose icosapent ethyl, a highly purified and stable EPA taken b.i.d., significantly reduced the risk of ischaemic events, including CV death, by about one-quarter over a median follow-up of 4.9 years. In addition, the VITAL trial showed that n-3 fatty acids at the lower dose of 1 g/day were not effective for primary prevention of CV or cancer events among healthy middle-aged men and women over 5 years of follow-up. Recommendations for the treatment of HTG are shown below.
Recommendations for drug treatment of patients with hypertriglyceridaemia
Monitoring Response To Therapy
Based on high-quality RCTs, fasting lipid measurement should be repeated four to 12 weeks after starting the statin or making a dose adjustment to assess adherence and response to LDL-Clowering medications and lifestyle changes. Following that, lipid measurement should be repeated every three to 12 months as needed.
Read Also: Does Tuna Have Cholesterol
Lifestyle Modifications To Improve The Plasma Lipid Profile
The pivotal role of nutrition in the prevention of ASCVD has been extensively reviewed. Dietary factors influence the development of CVD either directly or through their action on traditional risk factors, such as plasma lipids, BP, or glucose levels.
Convincing evidence of the causal association between diet and ASCVD risk is, nevertheless, available indirectly from randomized metabolic ward studies showing that high saturated fat intake causes increased LDL-C concentrations, and from cohort studies, genetic epidemiological studies, and randomized trials showing that higher LDL-C levels cause ASCVD.
The lack of concordance between studies is due both to methodological problems and the difficulties of evaluating the impact of a single dietary factor independently of any other changes in the diet. In fact, as foods are mixtures of different nutrients and other components, it is not appropriate to attribute the health effects of a food to only one of its components. Moreover, if energy intake must be kept constant, eating less of one macronutrient implies necessarily eating more of others. The quality of the replacement can influence the effect observed, significantly modifying the impact on health of the nutrient replaced. These limitations suggest caution in interpreting the results of RCTs or even meta-analyses of RCTs in relation to the effect of a single dietary change on ASCVD.
While The Guidelines Dont Recommend A Specific Target For Treatment They Do Suggest Additional Therapy In High
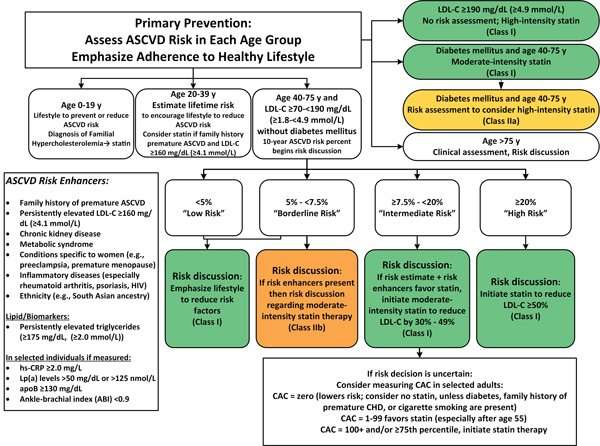
CHICAGO, IL New cholesterol guidelines from the American College of Cardiology and American Heart Association break ground by recommending ezetimibe and/or PCSK9 inhibition in selective high-risk patients and proposing noninvasive coronary artery calcium screening to help make decisions about patients who fall into the gray zone for treatment.
Presented today at the AHA 2018 Scientific Sessions, the new guidelines121 pages in length and 18 months in the makinginclude 72 recommendations, including 29 that are class I. In general, the ACC/AHA guidelines include a broad spectrum of support from numerous societies and recommend a heart-healthy lifestyle across the entire life span.
Richard Kovacs, MD , vice president of the ACC, said the latest guidelines will help transform cardiovascular care and improve heart health. High cholesterol is both often preventable and eminently treatable, but as we move into an era where care is personalized, how we treat individual patients can vary, said Kovacs. This guideline will give clinicians the tools that we need to have those conversations with patients about the most appropriate treatment for their high cholesterol.
While there is no target for ideal LDL cholesterol levels in the general population, the guideline recognizes, in principle, that lower is better. Ivor Benjamin
Whats New in the Secondary Prevention Setting?
In other words, the most intensive LDL-lowering is reserved for those at the highest risk. Neil Stone
Read Also: Does Shrimp Have High Cholesterol
Signs Symptoms And Complications
High bad LDL cholesterol usually does not cause symptoms, so most people do not know they have it until they are tested during a routine doctors visit. Very high levels may cause symptoms such as fatty bumps on your skin, called xanthomas, or grayish-white rings around the corneas in your eye, called corneal arcus. These mostly develop in people who have familial hypercholesterolemia.
Undiagnosed or untreated high blood cholesterol can lead to serious problems, such as heart attack and stroke.
Family History And Genetics
Family members usually have similar cholesterol levels. This suggests that your genes can raise your risk of having unhealthy cholesterol levels.
In addition, your genes may raise your risk for another type of bad cholesterol. High levels of lipoprotein-a, also called Lp, may mean you are at high risk of heart or blood vessel diseases, even if your other cholesterol levels are healthy. Genes determine how much Lp you have. Your Lp level is unlikely to change much from childhood to old age.
Lp is not usually part of a routine lipid panel. Your doctor may order an Lp test if you have a family history of early heart or blood vessel disease, such as heart attack, or do not know your family medical history. If you have a high Lp level, your doctor may prescribe a statin to prevent heart and blood vessel disease, even if your other cholesterol levels are in the healthy range.
Also Check: Shrimp And Cholesterol
What Happens During A Cholesterol Test
The cholesterol test, or screening, requires a simple blood draw. You may need to fast for 8 to 12 hours before your cholesterol test. Be sure to ask your doctor how to prepare for the test.
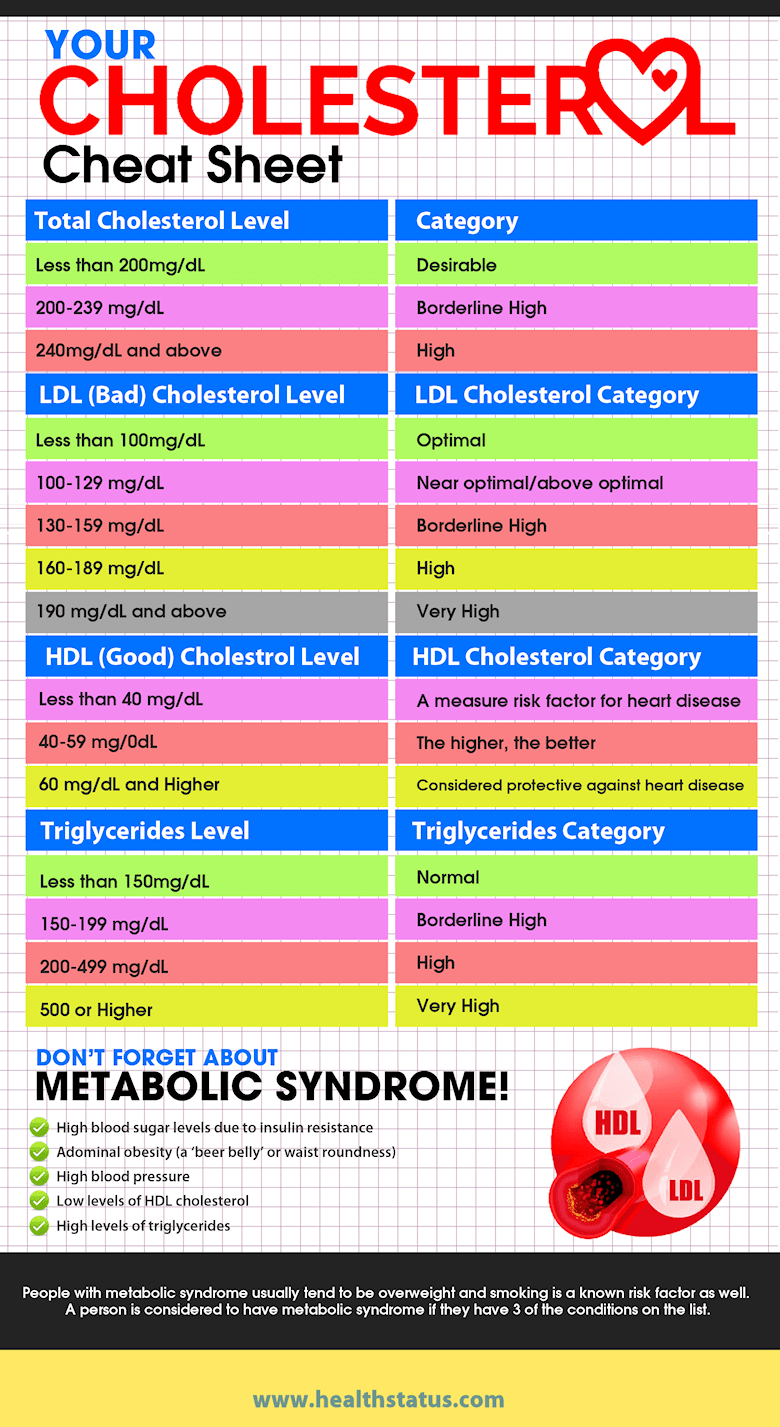
The cholesterol test checks your levels of:
- Low-density lipoprotein or badcholesterol. Having high levels of LDL cholesterol can lead to plaque buildup in your arteries and result in heart disease or stroke.
- High-density lipoprotein or goodcholesterol. HDL is known as good cholesterol because high levels can lower your risk of heart disease and stroke.
- Triglycerides, a type of fat in your blood that your body uses for energy. The combination of high levels of triglycerides with low HDL cholesterol or high LDL cholesterol levels can increase your risk for heart attack and stroke.
- Total cholesterol, the total amount of cholesterol in your blood based on your HDL, LDL, and triglycerides numbers.
Whats The Relationship Between Gender And Sex
Gender and sex can be related for some.
The expectation that if youre assigned male at birth, youre a man, and that if youre assigned female at birth, youre a woman, lines up for people who are cisgender.
But for people who are trans and gender non-conforming, the sex theyre assigned at birth may not align with the gender they know themselves to be. They may identify with a different sex than what they were assigned at birth.
Ultimately, the concepts of gender and sex are socially constructed. This means that we as a society assign sex and gender to people based on socially agreed-upon characteristics. This doesnt mean that body parts and functions are made up it just means that the way we categorize and define each of these things could actually be different.
People often like to separate gender and sex by saying things like gender is in the brain and sex is in the pants. Although accepting someone as their correct gender is a good first step, beliefs like these can actually be harmful to trans people.
When trans people are understood to be the sex they were assigned at birth and not the sex they truly are it can have a significant impact on their physical, mental, and emotional health.
For example, this can make it difficult to obtain fundamental rights, such as healthcare, and even access to basic necessities, such as public bathrooms.
Gender identity is your own personal understanding of your gender and how you want the world to see you.
Don’t Miss: Optilipid
Phytosterols And Liposoluble Vitamins
Considering that phytosterols reduce the intestinal absorption of cholesterol, itis reasonable to imagine that these substances may also reduce the absorption ofliposoluble vitamins and antioxidants. The serum levels of vitamins A, D, and K1are generally not affected by the consumption of phytosterols. However, some studies suggestthat phytosterols may promote a modest reduction in plasma concentration ofcarotenoids , and tocopherols, but other studies have notobserved this fact., A recently publishedmeta-analysis evaluated the effects of phytosterol consumption in plasmaconcentrations of liposoluble vitamins and carotenoids. It included 41randomized clinical trials with a mean phytosterol intake of 2.5g/day. In the analyses adjusted for total cholesterol, there was a significantreduction in the concentration of hydrocarbon carotenoids and some oxygenated carotenoids . In contrast, there was no significant reduction in theconcentration of tocopherol, vitamin D, or retinol. A very important finding ofthis meta-analysis was that the concentration of these substances remainedwithin the normal range, giving no indication that the observed reductions couldhave negative health implications. Noakes et al.have demonstrated that it is possible to avoid reductions inplasma carotenoid concentrations during the consumption of phytosterols throughan increase in daily consumption of carotenoid-rich fruits and vegetables.
What About Healthy People With Moderately Elevated Cholesterol Levels
What about healthy people who dont fit into the above categories? The guidelines provide clear guidance, but things do get a bit more nuanced. Here, there really needs to be a discussion between the patient and their doctor.
Whether to start a statin or not depends on whether there are other cardiovascular risk factors, such as smoking, high blood pressure, or diabetes, and the actual LDL-C level. A family history of premature atherosclerotic cardiovascular disease would be another factor to consider, as might South Asian ethnicity or premature menopause . Other blood test abnormalities, such as elevated triglycerides or elevated high-sensitivity C-reactive protein levels , might also push towards starting someone on a statin. Another recommendation in the new guidelines is for potential use of coronary artery calcium scans to decide whether or not to initiate statin therapy in select cases where the decision based on clinical risk factors is unclear. Patient preferences and cost are other potential issues to weigh. Online risk calculators may help.
Bottom line: If you are one of the large number of people who fall into this category, talk to your doctor about whether you should be on medications to lower your cholesterol, or whether lifestyle changes are enough.
Follow me on Twitter
Read Also: Is Bone Marrow High In Cholesterol
Risk Assessment Of Individuals With Diabetes
A detailed overview of risk assessment to guide decisions in whom to use statin therapy is provided in the Cardiovascular Protection in People with Diabetes chapter, p. S162. Principles of risk assessment also are discussed in the 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia , and efforts were made to ensure consistency between the guidelines. Accordingly, actual risk calculation is not required in most cases as people with diabetes > 40 years of age, or > 30 years of age and duration of diabetes > 15 years or with concomitant microvascular or cardiovascular disease warrant therapy .
Laboratory Measurement Of Lipids And Lipoproteins
Measurement of lipids and lipoproteins is used to estimate the risk of ASCVD and guide therapeutic decision-making. Quantification of plasma lipids can be performed on whole plasma and quantification of lipoproteins can be achieved by measuring their protein component. Operationally, lipoproteins are classified based on their hydrated density .
5.4.1 Lipoprotein measurement
Given the central causal role of ApoB-containing lipoproteins in the initiation and progression of atherosclerosis, direct measurement of the circulating concentration of atherogenic ApoB-containing lipoproteins to both estimate risk and guide treatment decisions would be ideal. Because all ApoB-containing lipoproteinsincluding VLDL, TG-rich remnant particles, and LDLcontain a single ApoB molecule, quantitation of ApoB directly estimates the number of atherogenic particles in plasma.
Standardized, automated, accurate, and inexpensive methods to measure ApoB are available. Fasting is not required because even in the post-prandial state, ApoB48-containing chylomicrons typically represent < 1% of the total concentration of circulating ApoB-containing lipoproteins. Furthermore, the analytical performances of ApoB measurement methods are superior to the measurement or calculation of LDL-C and non-HDL-C.
5.4.2 Lipid measurements
Plasma LDL-C can be measured directly using enzymatic techniques or preparative ultracentrifugation, but in clinical medicine it is most often calculated using the Friedewald formula:
Read Also: Canned Tuna Cholesterol
Lipid Panel Tests To Screen For High Blood Cholesterol
A lipid panel usually measures total cholesterol, LDL cholesterol, and HDL cholesterol. Your test results may also show the level of non-HDL cholesterol, which includes all fats that raise your risk of heart and blood vessels diseases. It may also include a test for triglycerides.
Ask your doctor if you need to fast before a lipid panel. This means you do not eat or drink anything except water for 9 to 12 hours before your visit. Ask your doctor about taking your medicines before the test.
How often you get a lipid panel done depends on your age, risk factors, and family history of high blood cholesterol or cardiovascular diseases, such as atherosclerosis, heart attack or stroke. Here is a general guide:
- Age 19 or younger. Screening begins at ages 9 to 11 and should be repeated every 5 years. Screening may be performed as early as age 2 if there is a family history of high blood cholesterol, heart attack, or stroke.
- Age 20 to 65. Younger adults should be screened every 5 years. Men ages 45 to 65 and women ages 55 to 65 should be screened every 1 to 2 years.
- Older than 65. Older adults should be screened every year.
Proprotein Convertase Subtilisin/kexin Type 9 Inhibitors
8.4.1 Mechanism of action
Recently, a new class of drugs, PCSK9 inhibitors, has become available that targets a protein involved in the control of the LDLR. Elevated concentration or function of this protein in plasma reduces LDLR expression by promoting, upon binding, LDLR lysosomal catabolism and a subsequent increase in plasma LDL concentrations, while lower concentration or function of PCSK9 is related to lower plasma LDL-C levels. Therapeutic strategies have been developed mainly using mAbs the mechanism of action relates to the reduction of the plasma level of PCSK9, which in turn is not available to bind the LDLR. Since this interaction triggers the intracellular degradation of the LDLR, lower levels of circulating PCSK9 will result in increased expression of LDLRs at the cell surface and therefore in a reduction of circulating LDL-C levels. Currently, the only approved PCSK9 inhibitors are two fully human mAbs, alirocumab and evolocumab. Statin treatment increases circulating PCSK9 serum levels, and thus the best effect of these mAbs has been demonstrated in combination with statins.
8.4.2 Effects on lipids
8.4.2.1 Low-density lipoprotein cholesterol.
8.4.2.2 Triglycerides and high-density lipoprotein cholesterol.
8.4.2.3 Lipoprotein.
8.4.3 Effect on cardiovascular morbidity and mortality
Early preliminary data from phase III trials suggests a reduction of CV events in line with the LDL-C reduction achieved.,,
8.4.4 Adverse effects and interactions
Also Check: Are Mussels High In Cholesterol
Lifestyle Recommendations To Improve The Plasma Lipid Profile
LDL-C lowering represents the primary target for reducing CV risk and therefore deserves special emphasis in the evaluation of lifestyle measures. The diet recommended to the general population, and particularly to people at increased CV risk, may also be able to modify plasma TG and HDL-C levels . This section focuses on dietary and other lifestyle factors that may be implemented to improve the overall lipoprotein profile.
7.4.1 Body weight and physical activity
Since overweight, obesity, andin particularabdominal adiposity often contribute to dyslipidaemia, caloric intake should be reduced and energy expenditure increased in those with excessive weight and/or abdominal adiposity.
In the case of excess weight, body weight reduction, even if modest , improves lipid abnormalities and favourably affects the other CV risk factors often present in dyslipidaemic individuals. While the beneficial effects of weight reduction on metabolic and surrogate markers have been demonstrated, the benefits of weight loss on mortality and CV outcome are less clear.
7.4.2 Dietary fat
Avoiding any consumption of trans fat is a key measure of the dietary prevention of CVD. The trans fatty acids produced in the partial hydrogenation of vegetable oils account for 80% of total intake. Thanks to efforts made in different parts of the world, the intake of trans fatty acids has decreased substantially over the past 1015 years.
7.4.3 Dietary carbohydrate and fibre
7.4.4 Alcohol
7.4.5 Smoking
What Are The Benefits And Risks Of Cholesterol Medications
Drug therapy is quite effective at reducing levels of cholesterol, according to the experts.
Statin medication has been shown to be very safe for the overwhelming majority of patients, Green said. Some patients report muscle weakness or discomfort that precludes their use. Liver enzymes are typically monitored while taking a statin medication, but risk of liver damage is extremely low.
Muscle aches or cramps are rare and are usually completely reversed with stopping the statin, Huang added. And though it depends on ones individual insurance plan, these drugs are the most affordable, as they are the standard treatments for cholesterol, Cornwell said.
PCSK9 inhibitors, a newer class of injectable cholesterol-lowering medications, have been shown to be very safe and tolerated well by the vast majority of patients, Green said. But they are also very costly: $15,000 to $20,000 per year. However, because of demand, Huang said the drug companies are cutting prices by as much as 60 percent. When combined with statins, these inhibitors have shown drastic reduction in LDL levels.
Using a cholesterol-reducing drug may be effective in reducing risk, but it may take time, Cornwell said.
The effects are not immediate, he said. Therefore, for older individuals, whose predicted lifespan is not more than a couple years, a practitioner could reasonably defer treatment because it would expose the individual to risks, like cost and side effects, without any immediate benefit.
Recommended Reading: Are Baked Potatoes High In Cholesterol