The Work Of Weston Price: Its Enduring Value
Weston Price promoted two theories about the relationship of nutrition and oral health to degenerative disease, which have long been ignored but have more recently gained support. In his earlier career, Price conducted 25 years of research demonstrating the ability of oral pathogens to cause cardiovascular and other systemic diseases. His work focused primarily on the tendency of the root canal procedure to facilitate this process.45 In his classic work on nutrition, Nutrition and Physical Degeneration, he connected nutritional status during development to deformities of the oral palate as well as to the risk of tuberculosis. Price believed that developmental deformities of the chest cavityproduced by the same nutritional causes as the deformities of the oral palatemade a person more vulnerable to the tuberculosis bacterium. For these reasons, he placed a special emphasis on the importance of nutritional preparation for and support of pregnancy and lactationpractices he universally observed among the healthy indigenous groups he studied.2 Modern science is now rediscovering the links between vascular disease and oral health and fetal nutrition.
How Does Atherosclerosis Affect My Body
Atherosclerosis is the primary cause of cardiovascular disease. Heart disease is the second leading cause of death in Canada. Types of cardiovascular disease include:
- Coronary artery disease: Coronary artery disease occurs when plaque builds up in the arteries that supply blood to your heart. When blood flow to your heart muscle slows or when the arteries become blocked, it can cause chest pain and heart attack.
- Small vessel disease: Small vessel disease occurs when plaque builds up in the small blood vessels of your heart. This can weaken your heart and cause chest pain, especially during exercise.
- Stroke: A stroke occurs when an artery that carries blood to your brain becomes blocked. This can cause temporary or permanent brain damage, and you may lose the ability to see, speak or to move parts of your body.
- Peripheral arterial disease : PAD occurs when plaque builds up in the arteries that supply blood to your arms or legs. This can cause numbness, pain and possibly infection in your affected limb.
Cholesterol Does Not Correlate With Degree Of Coronary Calcification
In contrast to conventional angiography, electron beam angiography detects coronary plaques independent of their location in the vessel wall, but only calcified plaques. Degree of coronary calcification seems a good surrogate for degree of coronary atherosclerosis, because it correlates strongly with total plaque volume and obstructive coronary disease, and is a powerful predictor of clinical outcome. Nonetheless, degree of coronary calcification did not correlate with any lipid fraction in the blood.
Read Also: What Is Average Cholesterol Range
Evidence From Mendelian Randomization Studies
Although the association between LDL-C and the risk of ASCVD is strong, graded, and reproducible in meta-analyses of prospective cohort studies, these studies are not randomized and are therefore unavoidably vulnerable to confounding, reverse causation, and other forms of bias. Mendelian randomization studies introduce a randomization scheme into an observational study specifically to assess whether an observed association between an exposure and an outcome is likely to be causal.
Numerous variants in multiple genes have been reported to be associated with lower LDL-C levels., Each of these variants is inherited approximately randomly at the time of conception in a process sometimes referred to as Mendelian randomization. Therefore, inheriting an LDL-C lowering allele in one of these genes is analogous to being randomly allocated to treatment with an LDL-C-lowering therapy, while inheriting the other allele is analogous to being randomly allocated to usual care. If the variant under study is associated solely with LDL-C and not with other lipid or non-lipid pleiotropic effects, and if allocation is indeed random, then comparing the risk of ASCVD among persons with and without such a variant should provide an unconfounded estimate of the causal effect of lower LDL-C levels on the risk of ASCVD in a manner analogous to a long-term randomized trial.
Cholesterol Does Not Predict Degree Of Atherosclerosis At Autopsy
In 1936, Landé and Sperry noted that the degree of aortic atherosclerosis at autopsy of healthy individuals who had died violently, was independent on their blood cholesterol concentration analysed immediately after death. Their finding was confirmed by Mathur et al. and similar results were obtained by others. The objection that an analysis of cholesterol after death may not reflect its concentration during life was met by Mathur et al. who found that the cholesterol concentration was almost constant up to 16h after death. Paterson et al. bypassed the problem by comparing the degree of atherosclerosis at death with the individuals cholesterol measured previously on several occasions. In all these studies, plots of blood cholesterol concentrations vs. the lipid content of the aorta or the coronary arteries were widely scattered.
More recent autopsy studies have found weak or inconsistent correlations between LDLcholesterol or total cholesterol and various measures of atherosclerosis. For instance, the most severe degree of atherosclerosis was found mainly in individuals with extremely high cholesterol, whereas small differences were seen in the rest. A correlation was found in White men, but not in Black men, in men but not in women, in individuals below, but not above age 80 years, and in the coronary arteries, but not in the thoracic or abdominal aorta.
Read Also: How Much Mg Of Cholesterol A Day
Atherosclerosis In Cardiovascular Disease
As the underlying cause of heart attack, stroke, and peripheral vascular disease, atherosclerosis is the major cause of death and morbidity in the United States and the industrial world . The discovery by Virchow more than 100 years ago that atheroma contained a yellow fatty substance, later identified as cholesterol by Windaus, suggested a role for lipids in the pathogenesis of atherosclerosis . Indeed, the goal of this chapter is to focus on the role of lipids and lipoproteins in the pathogenesis of atherosclerosis as well as their critical roles in risk assessment and as targets of therapy. The recognition that atherosclerosis is an inflammatory disease has led to tremendous progress in our understanding of the pathogenesis of atherosclerosis . First, we provide brief description of the cellular and molecular events in the key stages of atherosclerosis.
Hypertriglyceridemia As An Independent Risk Factor For Cardiovascular Disease
Meta-analyses of randomized, prospective trials probably provide the strongest evidence for triglyceride levels as an independent risk factor. One such analysis assessing the effects of lowering circulating cholesterol levels with statins, indicated that in patients with preexisting coronary heart disease, there was a reduction in residual risk not associated with lowering LDL-C that could be related to other lipoproteins, such as triglyceride-rich lipoproteins . Most convincingly, a recent meta-analysis of 29 prospective studies showed that considering triglyceride concentrations yielded an adjusted odds ratio of 1.72 for those in the top tertile of triglyceride levels even after adjusting for other common risk factors . A similar odds ratio was reported in a meta-analysis that included data from 26 prospective studies in Asian and Pacific populations .
Thus, the evidence is mounting for an independent role of circulating triglyceride levels in mediating cardiovascular risk and certainly has established the utility of determining triglyceride levels in at-risk patients. However, the studies also suggest that the association between high triglycerides and cardiovascular disease is complicated, multidimensional, and possibly indirect.
You May Like: What Do My Cholesterol Numbers Mean
The Common Good And Bad Cholesterol Levels Myth Is Not True
We have all heard over the course of the last several decades that ones cholesterol level predicts their risk of heart attack and stroke. Patients frequently ask me, How could I have heart disease my cholesterol level is normal? or report to me, I dont have to worry because my good cholesterol is high. As a cardiologist, I have both bad and good news: Your cholesterol level does not matter!
As you likely already know, cholesterol is a type of fat found within all cells and is free floating in blood on molecules called lipoproteins. The two most common of these lipoproteins containing cholesterol are low-density lipoprotein which carries cholesterol to the tissues , and high-density lipoprotein which carries cholesterol to the liver to be flushed from the body .
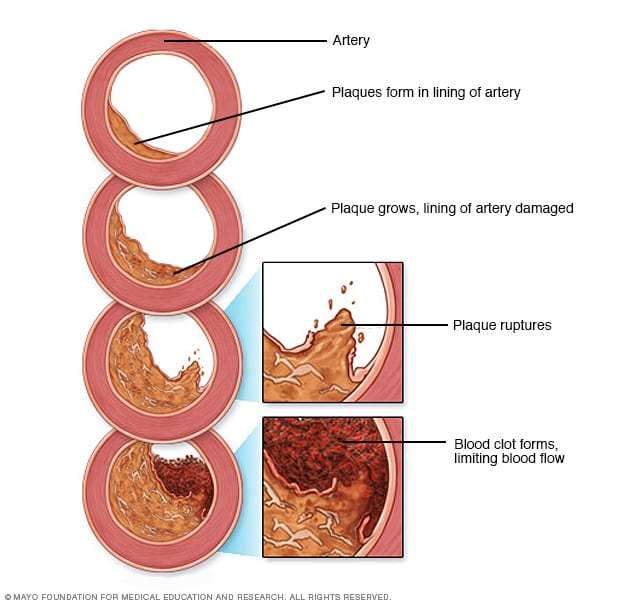
Cholesterol carried by LDL can invade the walls of blood vessels and lead to inflammation within the walls of these blood vessels. Cholesterol in this way forms the main constituent of plaque which builds up within the walls of blood vessels, in particular within the walls of arteries which carry oxygen-containing blood to the organs such as your heart and brain. This plaque can increase in size to eventually lead to a clogged artery, or the plaque can rupture which causes the blood near the ruptured plaque to clot. In the heart, these situations lead to chest pain , shortness of breath, or a heart attack. In the head and neck, clogging or obstruction of an artery leads to stroke.
Colchicine Potential Cardiovascular Benefits After Heart Attack
Inflammation plays a role in the development and progression of atherosclerosis and complications thereof, such as heart attack and stroke. Colchicine, an anti-inflammatory drug used to treat gout and familial Mediterranean fever, is often used off-label to treat pericarditis, a condition in which supportive tissue surrounding the heart muscle becomes inflamed.
A randomized controlled trial called the Colchicine Cardiovascular Outcomes Trial , published in late 2019, assessed the benefits of colchicine in people who had had a heart attack within the past 30 days.213 Participants received either 0.5 mg of colchicine or placebo daily and were followed-up for a median of nearly 23 months. A total of 4,745 participants were randomized in the study. The primary endpoint was a composite of death due to cardiovascular causes, resuscitated cardiac arrest, heart attack, stroke, or urgent hospitalization for chest pain leading to coronary revascularization. The composite outcome occurred less frequently among subjects randomized to colchicine. Specifically, the endpoint occurred in 7.1% of subjects taking placebo and 5.5% of those taking colchicine. The overall composite reduction with colchicine was driven largely by pronounced reductions in incidence of stroke and urgent hospitalizations for chest pain requiring coronary revascularization.
Recommended Reading: What Happens When Your Cholesterol Is Low
How Atherosclerosis Develops
Atherosclerosis develops over many years. During the course of the disease, several changes occur in the arteries, culminating in arterial plaques that may rupture and cause major cardiovascular events such as heart attack or stroke.11
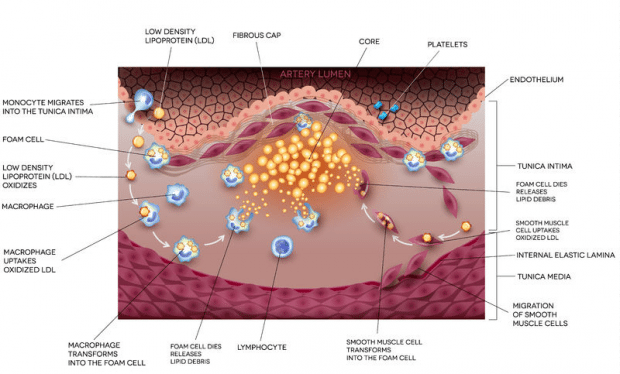
Endothelial cells are critical to the health and function of blood vessels. They line the inside of vessels and help facilitate healthy blood flow. In atherosclerosis, injury causes the endothelial cells to become dysfunctional and produce proteins that attract circulating immune cells called monocytes. The monocytes enter the blood vessel lining and transform into macrophages. Macrophages are specialized cells whose role is to engulf and destroy infectious agents, cancer cells, or other unhealthy substances. The macrophages become so-called foam cells by absorbing excess fatty deposits on the blood vessel walls, including low-density lipoproteins . As macrophages become filled with lipids, they develop a foamy appearance.12,13
Foam cells can also derive from vascular smooth muscle cells, which exist in normal blood vessels just below the endothelium and are responsible for contraction and relaxation of blood vessels. They can change their cell type to become more like macrophages and, ultimately, foam cells.14
How Low Can It Go
Early trials with cholesterol-lowering drugs were less than promising. A 1993 report pooled together the results of 13 trials conducted between 1966 and 1992 involving over 45,000 men. Cholesterol lowering had no effect on the incidence of stroke. There was a general tendency for it to decrease the risk of nonfatal stroke and increase the risk of fatal stroke, but the only trials in which the magnitudes of these differences were strong enough to be distinguished from the effects of chance were those that used the drug clofibrate. Clofibrate belongs to a class of drugs, called fibrates, that increase the excretion of lipids into the bile. Treatment with clofibrate more than doubled the risk of fatal stroke. The only trial that specifically reported the effect of treatment on hemorrhagic stroke used another fibrate called gemfibrozil. Treatment with this drug resulted in five times the risk of fatal hemorrhagic stroke.25
Hemorrhagic stroke is four times as deadly as ischemic stroke,21 and survival of both types is positively associated with cholesterol levels.22 The results of the early trials with cholesterol-lowering drugs may well reflect a tradeoff between hemorrhagic and ischemic stroke as well as a decreased ability to survive either type.
Recommended Reading: How Quickly Can You Lower Cholesterol
Renal Artery Stenosis Hypertension And Cholesterol
Renovascular hypertension is about 5% of all hypertension cases. In the presence of peripheral artery disease, the frequency of renal artery stenosis reaches up to 14%. There is an increase in the frequency of renal artery stenosis and peripheral artery disease association in the presence of diffuse peripheral artery disease . Atherosclerotic renal artery disease is the most common cause of renovascular hypertension. Atherosclerotic renal artery disease is often defined as having 60% stenosis in the osteal or proximal one-third of the renal artery. The second most common cause is fibromuscular dysplasia in younger individuals with no atherosclerotic risk factors. There is a string of beats view at the distal one-third of the renal artery. Renal artery stenosis can be tolerated by autoregulation mechanisms until the renal perfusion pressure reaches 70;mmHg. Renal revascularization has not been shown to reduce hypertension, renal, or cardiovascular events. Antihypertensive therapy, antiplatelet therapy, and statins are the main treatments.
Age And Family History
Aging is the dominant risk factor for clinically significant atherosclerotic lesion formation.44 Risk increases after age 45 in men and 55 in women. Plaque buildup that has been occurring for many years as a result of genetic factors, poor diet, and lack of physical activity may begin to cause health problems during middle-age.27
Family history is also an important risk factor for atherosclerosis, as an individuals risk increases if their father or brother was diagnosed with heart disease before age 55 or if their mother or sister was diagnosed before age 65.27 A prospective trial with over 5,000 subjects found that a family history of premature coronary heart disease is associated with the progression of coronary artery calcification. The greatest risk was with a combined parent and sibling history.45
Recommended Reading: Can Keto Cause High Cholesterol
Reducing Circulating Triglyceride Levels
It is clear, therefore, that there are a variety of ways in which the triglyceride-containing particles in hypertriglyceridemic plasma could contribute either directly or indirectly to multiple aspects of atherosclerotic lesion development. Regardless of whether triglycerides are directly causative of cardiovascular disease, the evidence is mounting that assessment of triglyceride levels has an important role in evaluating and managing cardiovascular risk, and treating elevated triglyceride levels may reduce risk for cardiovascular events . This is particularly true for patients with coronary heart disease or diabetes . Several agents have shown efficacy in reducing triglyceride levels and also in reducing cardiovascular disease risk. The reduced risk is thought to occur to a large extent by reducing atherosclerosis. Currently, therapeutic agents recommended for treating hypertriglyceridemia are fibrates, statins, niacin and omega-3 PUFA but others are being developed. Unfortunately, clinical trials of the impact of triglyceride lowering medications on cardiovascular events in subjects with severe hypertriglyceridemia have not been undertaken.
Drugs And Lifestyle Changes To Cut The Chance Of Having Atherosclerosis
Reducing the risk factors that lead to atherosclerosis will slow or stop the process. Ways to lower the amount of cholesterol in your body involve taking cholesterol and blood pressure medications, eating a healthy diet, getting frequent exercise, and not smoking. These treatments won’t unclog arteries. But they do lower the risk of heart attacks and strokes.
Lifestyle tips
Here is some advice that can help you improve your cholesterol level and reduce the risks that come with atherosclerosis:
- Exercise, with or without weight loss, increases “good” HDL cholesterol and reduces the risk of heart attacks and strokes.
- A diet high in fiber and low in fats can lower “bad” LDL cholesterol.
- Oily fish and other foods high in omega-3 fatty acids can raise âgoodâ HDL cholesterol.
- If you know or think your cholesterol is high, or if you have a family history of high cholesterol, talk to your doctor about ways you can lower it.
Medications
Statins are the most frequently prescribed cholesterol-lowering drugs. They can dramatically lower “bad” LDL cholesterol, by 60% or more. They can also increase HDL. Studies have shown that statins can reduce the rates of heart attacks, strokes, and death from atherosclerosis.
Statins can also help lower the level of triglycerides. Triglycerides are not cholesterol, but they are fats that contribute to atherosclerosis.
Statins include:
Fibrates
Bile acid sequestrants
Other drugs for lower cholesterol
Also Check: Does Skim Milk Have Cholesterol
A Convenient Choice Of Words
On February 20, 2007, Science Daily reported that researchers had shown total cholesterol levels to predict the risk of stroke in women. Women with the highest cholesterol levels, according to the article, had twice the risk of stroke as women with lower levels. The researchers claimed their findings underscored the importance of cholesterol levels as a risk factor for stroke, even if you have no history of heart disease and are otherwise healthy.8
The article left out one important fact: the study only looked at ischemic stroke.24 Did the women with high cholesterol levels have not only twice the risk of ischemic stroke but also half the risk of the much more dangerous and fatal hemorrhagic stroke? Was the incidence of total stroke any higher or lower in women with high cholesterol levels? We simply do not know; the study did not address the question.
What Is The Role Of Lipids In Atherosclerosis And How Low Should We Decrease Lipid Levels
Dr. Konstantinos C. Koskinas ,FESC
Retention of apolipoprotein-B-containing lipoproteins within the arterial wall is the key initiating event in the pathobiology of atherosclerosis. Consistent evidence from genetic studies, epidemiologic observations, and randomised controlled trials has unequivocally shown that elevated plasma concentrations of atherogenic lipid are causally linked to atherosclerotic cardiovascular disease, and that lowering these levels substantially reduces the risk of first or recurrent cardiovascular events. This article will focus on the role of lipids in the development of atherosclerosis and summarise currently recommended targets for lipid-lowering treatment as a means of reducing cardiovascular risk.
Read Also: Does Exercise Affect Cholesterol Test